Frequently Asked Questions about IBS Diet and Symptom Management
This article provides comprehensive information on the management of Irritable Bowel Syndrome (IBS). It covers an analysis of food categories that may trigger or alleviate symptoms, discusses the role and research status of supplements such as peppermint oil and certain probiotics, and provides general dietary management guidelines for special populations such as children. All information is compiled based on publicly available medical data and dietary research, aiming to enhance understanding, and should not replace professional medical diagnosis or personalized treatment plans.
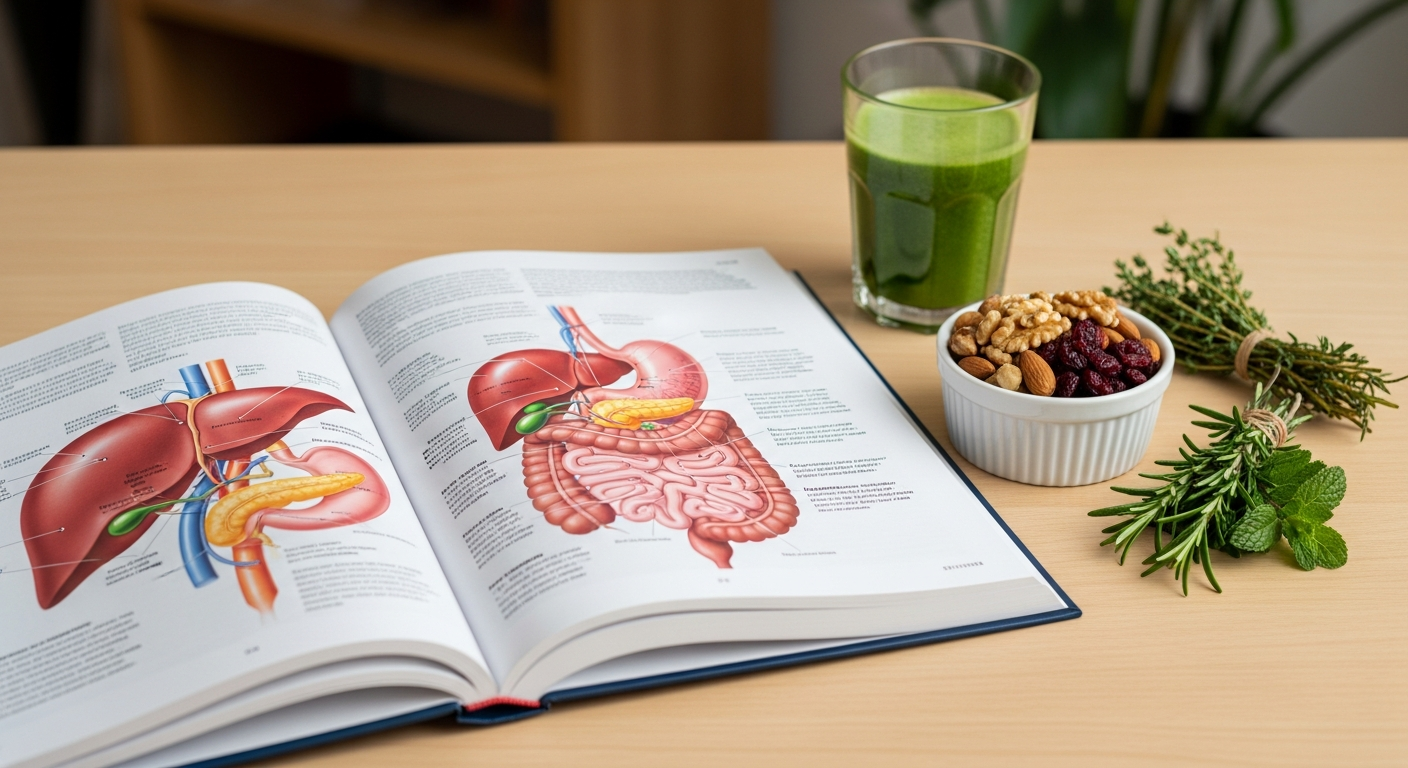
Irritable Bowel Syndrome affects millions of Americans, causing a range of uncomfortable digestive symptoms that can significantly impact quality of life. While there is no one-size-fits-all cure, understanding how diet and lifestyle choices influence symptoms can provide meaningful relief. This article explores evidence-based approaches to managing IBS through nutrition, supplementation, and practical daily habits.
Analysis of Food Triggers and Relief Strategies for IBS Symptoms
Identifying food triggers is one of the most effective ways to manage IBS symptoms. Common culprits include high-FODMAP foods such as certain fruits, vegetables, dairy products, wheat, and legumes. FODMAPs are short-chain carbohydrates that ferment in the gut, producing gas and triggering symptoms like bloating, cramping, and altered bowel habits. Keeping a detailed food diary helps track which foods correlate with symptom flares. Many people find relief by following a low-FODMAP diet under the guidance of a registered dietitian. This approach involves eliminating high-FODMAP foods for several weeks, then systematically reintroducing them to identify personal triggers. Other common triggers include caffeine, alcohol, spicy foods, and high-fat meals. Relief strategies include eating smaller, more frequent meals, staying hydrated, and avoiding eating too quickly. Stress management techniques such as meditation, yoga, and regular exercise also play a crucial role in symptom control, as the gut-brain connection significantly influences IBS.
Information on the Role of Supplements such as Probiotics and Peppermint Oil
Supplements have gained attention as supportive tools for IBS management, though individual responses vary. Probiotics are beneficial bacteria that may help restore balance to the gut microbiome. Research suggests certain strains, particularly Bifidobacterium and Lactobacillus species, can reduce bloating, gas, and abdominal pain in some IBS patients. However, not all probiotics work the same way, and finding the right strain and dosage often requires trial and error. Peppermint oil is another well-studied supplement that has shown promise for IBS symptom relief. Enteric-coated peppermint oil capsules can help relax intestinal smooth muscle, reducing cramping and discomfort. Studies indicate it may be particularly effective for IBS with predominant abdominal pain. Other supplements sometimes recommended include fiber supplements like psyllium for constipation-predominant IBS, digestive enzymes, and vitamin D, especially in individuals with deficiencies. It is important to consult with a healthcare provider before starting any supplement regimen, as some may interact with medications or worsen certain symptoms.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
General Dietary Recommendations for Children with IBS
When children experience IBS symptoms, dietary management requires special consideration to ensure they receive adequate nutrition for growth and development. Parents should work closely with pediatric gastroenterologists and dietitians to create age-appropriate meal plans. The low-FODMAP diet can be adapted for children, but complete elimination should be temporary and carefully monitored to prevent nutritional deficiencies. Focus on providing balanced meals with lean proteins, well-tolerated fruits and vegetables, and whole grains that do not trigger symptoms. Encouraging regular meal times and avoiding rushed eating can help reduce digestive stress. Many children with IBS benefit from limiting carbonated beverages, excessive fruit juice, and processed snacks high in artificial sweeteners. Ensuring adequate fiber intake through tolerated sources supports healthy bowel function. Emotional support is equally important, as anxiety about symptoms can worsen the condition. Teaching children relaxation techniques and maintaining open communication about their symptoms helps them feel more in control. Regular follow-up with healthcare providers ensures dietary approaches remain effective and nutritionally complete as children grow.
Common Questions about Daily Dietary Management of IBS
Managing IBS on a daily basis involves developing sustainable eating habits that minimize symptoms while maintaining nutritional balance. One frequent question is whether meal timing matters. Evidence suggests eating at consistent times each day helps regulate digestive function and can reduce symptom unpredictability. Another common concern is dining out or social eating situations. Planning ahead by reviewing menus, communicating dietary needs to servers, and choosing simple preparations can make eating away from home less stressful. Many people wonder if they need to avoid entire food groups permanently. In most cases, complete avoidance is unnecessary once triggers are identified. The goal is finding personal tolerance levels rather than following overly restrictive diets. Hydration is another important factor. Drinking adequate water throughout the day supports digestive health, though some people find that drinking large amounts with meals worsens bloating. Alcohol and caffeine tolerance varies widely among IBS patients. Some can enjoy moderate amounts without issue, while others find these beverages consistently trigger symptoms. Food preparation methods also matter. Cooking vegetables until soft, choosing lean proteins, and limiting added fats can improve tolerability. Ultimately, successful daily management comes from understanding your individual patterns, being flexible, and recognizing that occasional symptom flares are normal and manageable.
Living with IBS requires patience, self-awareness, and a willingness to experiment with dietary and lifestyle modifications. While the condition can be challenging, many people find significant relief through identifying food triggers, incorporating helpful supplements, maintaining consistent eating patterns, and managing stress. Working with knowledgeable healthcare providers ensures that management strategies are safe, effective, and tailored to individual needs. With the right approach, it is possible to reduce symptom frequency and severity, leading to improved quality of life and greater confidence in daily activities.